NEW Research Confirms the UK’s Current Salt Reduction Programme is No Longer Fit for Purpose
NEW research from Queen Mary University London published today (19.09.2023) in the Journal of Hypertension[i], shows the Government has failed to reduce population salt intakes and consequently improve public health in England since 2014 when the UK’s successful salt reduction programme was handed directly to the food industry – putting thousands of lives at risk.
Today, Action on Salt together with 33 leading experts and health charities[ii] are calling on party leaders to prioritise salt reduction through a mandatory and comprehensive programme. Failure to act will have a detrimental impact on the health and wellbeing of the population, as well as on the economy.
Open Letter to Rishi Sunak [PDF 199KB]
Open Letter to Sir Keir Starmer [PDF 211KB]
This also coincides with a NEW consumer poll[iii] by Action on Salt which shows nearly 90% of the UK population would support the government in taking action to protect the public from avoidable health conditions like heart disease and strokes whilst nearly 80% think ministers should do more to reduce the salt we eat as a nation. Furthermore, 85% of the population would support the government in requiring food companies to reduce unnecessary salt in their products.
This latest published research (Salt Intake, Blood Pressure and Cardiovascular Disease Mortality in England, 2003- 2018) aimed to investigate the impact of the UK’s pioneering voluntary salt reduction programme since its inception. Using publicly available data[iv] to evaluate population salt intake, blood pressure (BP) and deaths from heart disease and stroke, the results showed that whilst average salt intake, BP and deaths in the adult population of England initially decreased as a result of the pre-2014 policies, the declines have since stopped:
- A decline in salt intake from 9.38g/day to 7.58g/day between 2003 and 2014, followed by an increase to 8.39g/day in 2018
- A decline in population BP from 125.3/74.5 mmHg to 122.6/73.3 mmHg between 2003 and 2014, following by a plateau 122.0/73.8 mmHg in 2018
- A fall in stroke and heart disease mortality rates from 12.2 and 43.4 deaths per 100,000 to 8.2 and 27.2 deaths per 100,000 between 2003 and 2014, followed by a plateau afterwards.
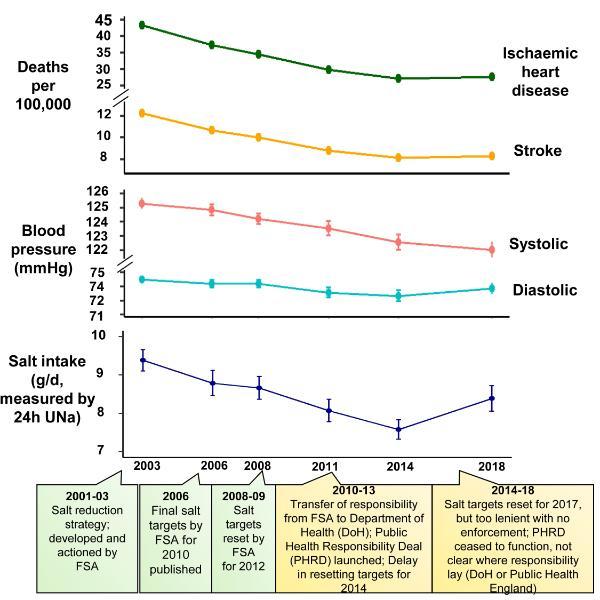
Figure 1. The salt reduction journey in England, from 2003 to 2018. Dietary salt intake, blood pressure and cardiovascular disease mortality, alongside key policy moments for salt reduction in the country.
These findings confirm an already overwhelming body of evidence linking the importance of salt reduction to improved health, and that when done correctly, a salt reduction programme can save thousands of premature deaths from strokes and heart disease. However, the lack of progress since 2014, coinciding with responsibility for the salt reduction programme being handed over to the food industry, indicates that the effectiveness of the programme has been compromised. It was estimated that, if the previous successful programme had continued, there would have been a further reduction of 1.45 g/day in salt intake from 2014 to 2018. This would have prevented over 38,000 deaths from strokes and heart disease in just a 4-year period, of which 24,000 would have been premature[v]. This research also provides valuable evidence for policymakers and public health authorities that comprehensive and well-managed salt reduction programmes, are pivotal in preventing strokes and heart disease events, two of the leading causes of death in the UK.
Professor Graham MacGregor, Professor of Cardiovascular Medicine at Queen Mary University of London, Chairman of Action on Salt and co-author of the analysis says: “This study reinforces the urgent need for a robust system where we generate worthwhile reductions in salt intake which make a positive and lasting impact. It is now up to the Government to set up a coherent strategy where the food industry is instructed what to do, rather than the food industry telling the Government what to do. We must get our salt reduction strategy back on track for the benefit of public health, the UK workforce, our overburdened NHS and the economy."
Jing Song at Queen Mary University of London and first author of the Journal of Hypertension analysis says: “Reducing salt intake has been identified by the World Health Organisation as one of the most cost-effective measures to improve population health. As a nation, if we cut one gram of salt from our average daily salt intake, this could save over 6,000 lives every year from strokes and heart disease - all of which are completely avoidable – and save the economy £1.5 billion annually."
Sonia Pombo, Campaign Lead at Action on Salt and co-author adds: “The once successful salt reduction programme is a shell of its former self. Salt reduction is simple and easy to implement, and this research confirms it works. But the UK’s downfall was trusting the food industry to deliver reductions in salt content without an incentive to do so or enforcement from the Government. Urgent resuscitation in the programme is needed if we are to get back on track and save the most lives.”
Edwina Revel, Programme Director at Early Start Nutrition, said: “In the early years it’s important to expose children to a wide range of tastes to develop their preferences which they’ll take into their adult years. It’s essential that babies and toddlers don’t develop a taste preference for salty foods as they’re more likely to eat salty foods as they grow up. A high salt diet can result in children developing high blood pressure. The higher the blood pressure in childhood, the higher it will be in adulthood, increasing their risk of heart disease in later life. As babies and toddlers take part in family meals they’re exposed to higher than recommended salt levels. Food quality matters for our youngest generation and we support Action on Salt in calling for both mandatory salt reduction targets and the introduction of a reinvigorated programme in the UK to prioritise salt reduction.”
Barbara Crowther, Children’s Food Campaign Manager at Sustain, said: “This is yet more evidence that, without a proper Government mandatory framework providing the incentive, progress towards healthier food is not going to be achieved. We’ve seen with the Soft Drinks Industry Levy how effective it can be when they do. Now Government needs similar ambitions to push companies harder to change the recipe on salty food. Doing so would protect the nation from a range of health conditions and support a healthier nation and economy.”
[i] Song J, Tan M, Wan C, Brown MK, Pombo-Rodrigues S, MacGregor GA, He FJ. Salt intake, blood pressure and cardiovascular disease mortality in England, 2003-2018. Journal of Hypertension 2023, 41:000–000 https://journals.lww.com/jhypertension/abstract/9900/salt_intake,_blood_pressure_and_cardiovascular.305.aspx
[ii] 33 leading experts and health charities have signed an open letter to Government Party leaders calling for a mandatory and comprehensive programme to reduce population salt intake. Charities include British Dietetics Association, British Heart Foundation, British Medical Association, Blood Pressure UK, Caroline Walker Trust, Chefs in Schools, Early Start Nutrition, Food Active, Food Foundation, Faculty of Public Health, First Steps Nutrition Trust, Heart UK, LEYF Nurseries, Nutrition Scotland, Obesity Health Alliance, PKD Charity, Royal Society of Public Health and Sustain.
[iii] The research was conducted by Censuswide with 2,001 UK nationally representative general respondents (16+) between 30.08.23 – 01.09.23. Censuswide abide by and employ members of the Market Research Society which is based on the ESOMAR principles and are members of The British Polling Council
[iv] Data from the National Diet and Nutrition Survey (NDNS), the Health Survey for England (HSE) and the National Office for Statistics was used to evaluate population salt intakes, blood pressure (BP) and deaths from heart disease and stroke. All data and materials have been made publicly available at the UK Data Service (https://beta.ukdataservice.ac.uk/datacatalogue/series/series?id=2000033, https://beta.ukdataservice.ac.uk/datacatalogue/series/series?id=2000021)
and Global Health Data Exchange (https://vizhub.healthdata.org/gbd-results)
[v] This equates to 9,600 deaths/year, of which 6,000 would have been premature. This is based on estimations from NICE’s report. Premature deaths is defined as deaths occurring before the age of 75


